Abstract
Aim:Though senior citizens of the same age have variable physical, cognitive functions and comorbidities, treatment decisions are still based on disease biology and chronological age. In our registry, 43% (95/219) patients stopped azacitidine (AZA) before completing six cycles and 80% of patients stopping AZA were aged ≥65 years of age. This prospective study assesses the feasibility of a multidimensional geriatric assessment (MGA) in the management of elderly MDS patients.
Method: After initial review by the haematologist to assign a treatment, patients underwent MGA conducted by trained nurse on consented patients. MGA was performed using well-defined tools: ECOG, ADL, iADL, GDS, mini-nutritional assessment (MNA), MMSE, falls risk and Charlson comorbidity index (CCI) and MDS-comorbidity index (MDS-CI). Patients that had abnormal scores were referred for Geriatrician review and appropriate allied health reviews. Recommendations were communicated to the treating physicians and general practitioner.
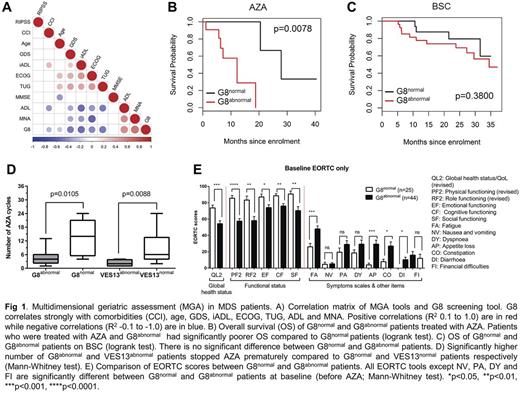
As MGA can take 80-90 minutes, two geriatric screening tools (VES-13 and G8) were also used. Patients were classified as G8abnormal (score ≤14), G8normal (score ≥15), VESabnormal (score ≥3) and VESnormal(<3). Sensitivity, specificity, positive (PPV) and negative (NPV) predictive value for detecting abnormalities on MGA were calculated. Correlation between G8, VES-13 and MGA domains was analysed using Spearman's correlation. Overall Survival (OS) was examined using Kaplan-Meier analyses, with significant differences between the two groups assessed using log-rank test
Results: Sixty-nine MDS patients ≥65 years had CGA assessment after treatment decision but before commencing treatment. Forty-eight (68%), 18 (26%) and 4 (6%) patients were treated with best supportive care (BSC), Azacitidine (AZA) and Lenalidomide respectively. Though ECOG was ≤1 in 51(75%) cases, 58(84%) patients had comorbidities, and 27(38%) and 21(31%) were dependent for iADL and ADL respectively. Importantly, iADL (p=0.008) and ADL (p<0.001) dependency was associated with signficantly poorer OS in AZA treated patients. Additionally, 37%, 26% and 13% patients were at higher risk of depression (GDS>5), malnutrition (MNA<23.5) and cognitive impairment (MMSE <24) respectively. Importantly, Cox regression analysis showed that high CCI (HR 2.6; p=0.04), and ADL (HR 0.02; p<0.001) and iADL (HR 10.7; p=0.001) dependency predicted poor prognosis independent of Revised International Prognostic Score (R-IPSS; HR 1.6; p=0.004).
Geriatric screening tools G8 and VES13 classified 45(64%) and 36(51%) patients at risk of frailty. As compared to VES-13, G8 was more senstive (75% vs. 91%) and has higher PPV (88% vs. 93%) and NPV (60% vs. 84%) in detecting at least two abnormalities on MGA. While specificity of both tools were similar (83% vs. 87%), G8 strongly correlated with ADL, iADL, GDS, MNA, Age and comorbidities (Fig 1A). Importantly, G8abnormal patients had signficantly poorer OS (12 vs. 28 months; p=0.008) in AZA treated patients but not in BSC group (Fig 1B-C). While VES-13 did not predict OS in both AZA and BSC patients. Additionally, signficantly higher number of G8abnormal (4.5±3.2 vs. 13.7±7.7; p=0.002) and VESabnormal (4.1±4.1 vs. 9.8±7.1; p=0.01) patients stopped AZA prematurely compared to G8normal and VESnormal patients respectively (Fig 1D), despite providing apporpraite support/interventions indicated by geriatric assessment. Quality of life assessed using EORTC tools was signficantly poorer in G8abnormal compared to G8normal patients. Global health status and functional status was signficantly poorer while symptom burden was higher in G8abnormal patients (Fig.1E).
Conclusion: Multidimensional geriatric assessment demonstrate that 84% of elderly MDS patients suffer with comorbidities and 38% patients are dependent for iADL. Comorbidities, ADL and iADL dependency is associated with signficantly poorer survival independent of IPSS-R. The geriatric screening tool G8 is sensitive, specific, has a high PPV and NPV in detecting abnormalities on MGA. More importantly, the finding that G8 predicts poor treatment completion rate, signficantly poor survival in AZA treated patients and is associated with poor QOL is previously unreported and novel. A formal geriatric assessment should be included in the treatment decision-making of elderly MDS patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal